As a woman of colour, I have the advantage of having less wrinkles as I age but am more prone to pigmentation. This is because of my melanin, the pigment that gives my skin my colour which is protective against wrinkles but as a sacrifice, increases my pigmentation.
In this blog, I wanted to dive deeper on why we get more pigmentation when we age and what treatment options are there available.
LET’S START WITH THE SCIENCE BEHIND PIGMENTATION
Skin pigmentation refers to how much melanin we have in our skin. Melanin produces the various shades and colour of the human skin, hair and eyes. Without melanin, the skin would be pale white with shades of pink caused by blood flow through the skin. Fair-skinned people produce very little melanin, darker-skinner people produce moderate amounts and very dark-skinned people produced the most.
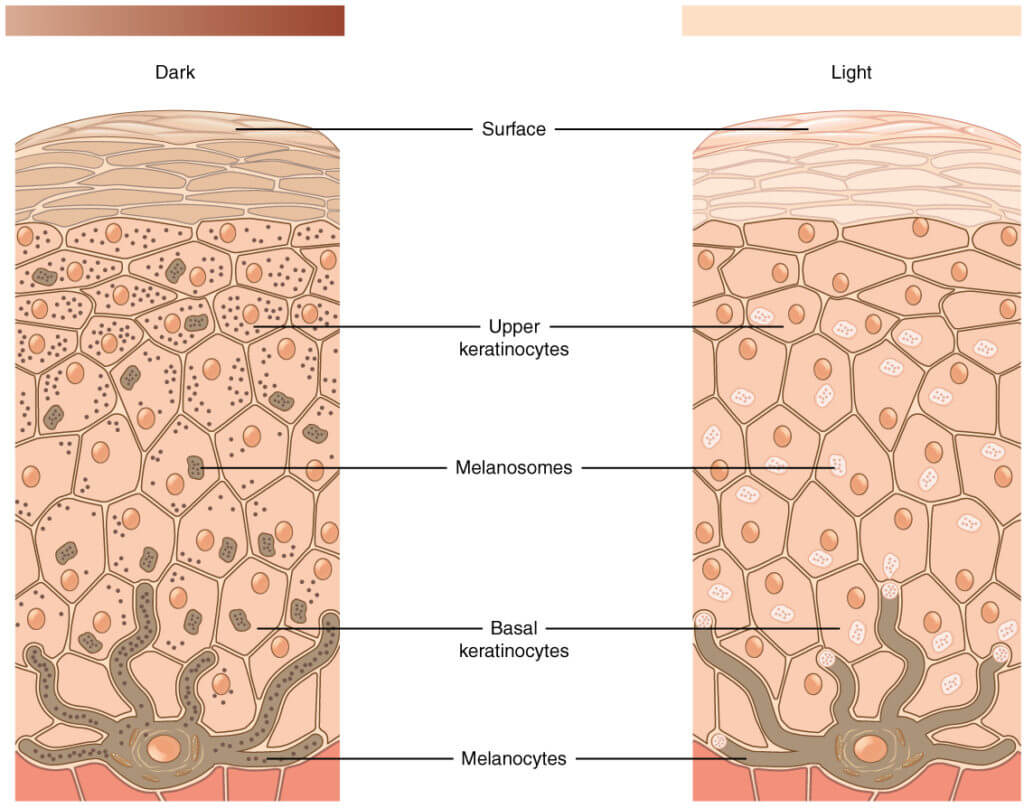
Melanin is the pigment produced by specialised cells called melanocytes in the deepest layer of the outer layer of the skin (epidermis) called the basal layer. Melanocyte looks a one-eyed octopus with arms (dendrites) reaching the cells above. After melanin is produced, it spreads into nearby cells transported by vesicles called melanosomes.
Melanin acts as a shield, serving as a physical barrier that scatters UV radiation and as an absorbent filter that reduces the penetration of UV through the epidermis. Hence why darker skin have less wrinkles. Usually, melanin is fairly evenly distributed in the skin, but sometimes people have spots or patches of skin with more melanin e.g. seen in freckles, birth marks, age spots lentigines or liver spots), melasma and post-inflammatory hyperpigmentation.
There are 3 types of pigmentation disorders:-
Depigmentation is complete loss of pigment. The skin is white. Widespread depigmentation occurs in vitiligo.
Hypopigmentation is an abnormally low amount of melanin. The skin is lighter in colour than normal. Widespread hypopigmentation occurs in albinism. It can also be caused by:-
- Previous injury to the skin, such as a blister, burn, ulcer, exposure to a chemical or skin infection.
- Inflammatory conditions of the skin that have healed such as atopic dermatitis or psoriasis.
- Rare hereditary conditions.
Hyperpigmentation is due to:
- an abnormally high amount of melanin
- concentrated distribution of melanin
- deposition of other pigmented substances that are not normally present in the skin
WHY DO WE GET MORE PIGMENTATION AS WE AGE?
1. Photoageing by excessive or accumulated exposure to the sun
The darker skin you are, the quicker you can tan. It’s a protective mechanism as melanin acts as a shield and physical barrier to UV radiation. The lighter skin you are, the higher chance of getting a sunburn.
UVA induces immediate tanning and persistent pigment darkening through oxidation of pre-existing melanin or precursors in the pathway to making melanin in the cells. UVB induces delayed tanning which takes several days or longer to develop and requires activation of melanocytes to produce more melanin.
This is seen in age spots (also known as sun spots, actinic lentigines or lives spots). They are flat, oval areas of increased pigmentation typically on back of the hands, forearm, tops of the feet, face, back of the neck, shoulders, upper back and chest. They do not progress to skin cancer and do not require treatment.
2. Hormonal changes such as pregnancy, perimenopause and menopause.
There are about 50 different types of hormones in a female body. I’m only touching on a small area.
The first hormone is Oestrogen which I now refer to as the Superwoman hormone. I will write a future blog on her. In the meantime, Oestrogen helps to maintain epidermal thickness and barrier function by stimulating production of collagen, ceramides and hyaluronic acid. It also stimulates melanocytes to produce more melanin and improve blood flow which can be seen as having “more colour” or “glow” during ovulation when it peaks to attract a mate.
Higher oestrogen levels as seen in pregnancy, if you’re on the combined pill and in the early phase of perimenopause (due to relatively low progesterone) can activate the melanocyte to produce more melanin. This is commonly presented as melasma.
Melasma can appear as light brown, dark brown or blue-grey blotch patches on the skin. It can be flat or freckle-like, usually on the cheeks, the forehead or above the lip. This is difficult to treat and usually returns.
The effects of oestrogen is counteract by progesterone which interestingly reduces melanin production, thereby reducing pigmentation.
However I need to highlight it’s all about balance because if there was only progesterone with no oestrogen, research has shown it can actually increase pigmentation too.
In menopause, oestrogen and progesterone declines dramatically. The skin becomes thinner and paler (due to less blood flow) so there is less protection against UV damage and the areas where pigments are concentrated can be more visible.
Increased pigmentation can also occur with increasing stress. This is due to the hormone ACTH (adrenocorticotrophic hormone) which is produced from the pituitary gland to regulate the hormone cortisol. This can be broken down to melanocyte-stimulating hormone which activates the melanocyte to produce more melanin.
As we age, our thyroid function generally declines, worsened by stress and low oestrogen. Thyroid hormone limits the growth of melanocytes which explains why people who are hypothyroid (too little thyroid hormones) are at a higher risk of developing melanoma, a form of skin cancer that starts in the melanocytes. Low thyroid can also affect the immune system, creating more inflammation, which increases melanin production.

3. Cellular senescence
I wrote about this in my pervious blog on Improving Skin Laxity.
Senescence is a state of permanent growth arrest so the cell is unable to proliferate and no longer able to contribute to tissue repair or regeneration. These cells are effectively “useless” which leads to inflammation and breakdown of the area by protective cells.
With chronological ageing, the number of functional melanocytes gradually declines and melanogenic activity is reduced, resulting in the appearance of pale skin in the elderly. However the melanocytes of photo exposed skin are relatively well-maintained most likely due to persistent UV stimulus affecting the melanocytes.
Melanocyte senescence is characterised by melanocytes with less dendrites so the pigments are not distributed to the cells above and instead concentrated in the body of the cells. With thinner skin as we age, this becomes more visible.
Senescence of neighbouring cells e.g. fibroblast and immune cells increases inflammation within these micro-environment, increasing pigmentation. Senescence of keratinocytes results in thinner skin, increasing UV exposure and visible pigmentation.
4. Drugs and Herbs
This occurs because certain drugs:-
- can directly increase melanin production.
- can accumulate in the skin.
- can make the skin more sensitive to the sun, increasing risk of photodamage
Potential drugs include:-
- chemotherapy medication
- antimalarials, antibiotics, antifungals
- non-steroidal anti-inflammatory drugs (NSAID) commonly used for joint pains
- antianxiety medication, antidepressants.
- amiodarone used to treat or prevent heart rhythm disorders
- anticonvulsants
- minocycline, an antibiotic normally used to treat STIs
- roaccutane used in acne
Drug-induced pigmentation occurs in all skin types and ethnicities but certain combinations of skin types and medications may experience more significant pigmentation effects. Somehow it’s more common in women and people of Asian or African descent.
Certain plants and herbs can also make the skin photosensitive, increasing the effects of ultraviolet e.g limes, celery, parsely applied topically.
5. Increase injury to the skin
Skin injury e.g. acne or cuts/burns with more fragile skin or after a rash increases post-inflammatory hyperpigmentation where melanin production is stimulated as part of the healing process.
6. Nutrient deficiency
Hyperpigmentation can also be seen in deficiency in Vitamin B12, folic acid, iron and Vitamin D. This could be due to reduced intake, problem with absorption or increased loss e.g. low iron from menstrual bleeding.
BEFORE WE EXPLORE TREATMENT OPTIONS
I want to make sure you know the 8 signs of potential skin cancer because if there is any suspicion, I want you to take your beautiful self to get it checked out by your GP or private dermatologist.
These are:
- New or changing spots that aren’t brown.
- Skin changes in odd places.
- A lesion that bleeds.
- A painful lesion.
- A lesion that itches.
- A spot with a crater-like appearance
- Rapid growth of a spot.
- A lesion that has irregular borders.

TREATMENT OPTIONS TO IMPROVE HYPERPIGMENTATION
From understanding the science behind pigmentation, we can improve it by:-
- Reducing factors that activate melanocytes (inflammation is a big one).
- Intercepting the pathway of making melanin in melanocytes (melanogenesis).
- Intercepting the delivery of melanin to the cells above.
- Removing superficial cells that contain these concentrated areas of melanin.
- Improving dermal thickness so pigmentation is less visible and the dendrites are “stretched out” so the pigments are deposited further away.
- Reducing cellular senescence
1. Topical creams
Skin brightening ingredients e.g. Vitamin C, kojic acid, arbutin, liquorice extract, azelaic acid, retinol and cysteamine all intercept melanogenesis in their own unique way so less pigment is made.
Niacinamide reduces the delivery of melanin to the cells above.
Retinoids also increase epidermal cell turnover, breaking up the concentrated pigments and dispersing it out. Hydroquinone reduces production of melanin and also selectively damages melanocytes and melanosomes.
There are MANY products with formulations of different ingredients. Protocols will depend on skin type, the intensity and distribution of the pigmentation and tolerability for down time. Stronger ingredients will require monitoring as can result in redness, dryness and skin peeling.
Epidermal pigmentation is easier to treat than dermal pigmentation.
Dermal pigmentation is in a deeper layer and is characterised by having a genetic predisposition, high melanin count and high vascular/ erythema. This is seen in melasma, post-inflammatory hyperpigmentation and solar lentigines (age spots due to photo ageing).
Pigmentation can potentially return if these ingredients are stopped as melanogenesis resume its normal function.
2. Resurfacing treatments
This removes the pigmented cells and also encourage dermal remodelling and rejuvenation. This can be done via 3 modalities:-
- Physical resurfacing using in-clinic microneedling and at home derma roller.
- Chemical resurfacing (skin peels) using glycolic acid, mandelic acid, salicylic acid, lactic acid or TCA.
- Energetic resurfacing using lasers.
You may require a few sessions and the results can be dramatic. However there is a higher risk of post-inflammatory pigmentation which can be mitigated by appropriate preparation of the skin before the treatment and suppressing melanogenic activity afterwards.
3. Broad band light (BBL) or Intense Pulse Light (IPL)
IPL and BBL uses light of different wavelengths which is selectively penetrated by the pigments which is then “destroyed” and dispersed from the skin.
IPL is more a generic term while BBL is the trademark name from the company, Sciton. BBL seem to be a popular choice among practitioners due to the design of the machine, giving better and more consistent results.
Unlike traditional lasers, which utilises a single colour of light, BBL flashes a whole spectrum of colours at a one time, utilising different wavelength (hence the term broad), thereby creating clearer and brighter skin. The light energy, also called photothermal energy is directed at the skin in short blasts of high-intensity light which focuses heat on these areas.
This will require at least 3-5 sessions for maximum results. There is minimal discomfort and downtime. This is “safer” than traditional lasers but still a risk for darker skin tones for PIH (post inflammatory hyperpigmentation).
4. Skin boosting treatments
I rave a lot about Sunekos, the best skin boosting treatment I have found because of how it works at a cellular level. Sunekos is a hyaluronic acid with a patented formulation of 6 amino acids. It acts differently than normal skin boosters because it not only stimulates but also optimises the cells.
It improves the quality and health of the skin so the melanocytes behave themselves and epidermal turnover increases, stretching the space between each dendrites and the pigments are stretched out, making it less intense and visible. Research have shown Sunekos reducing pigmentation by 50%.

5. Supplements
Supplements can help to reduce hyperpigmentation by:-
- improving immunity and reducing inflammation (e.g. Vitamin A and B’s)
- provide extra antioxidant cover (e.g. Vitamin C, Astaxanthin)
- repairing DNA (glutathione)
- reduce the skin’s susceptibility to damage by UV radiation (e.g. Omega 3)
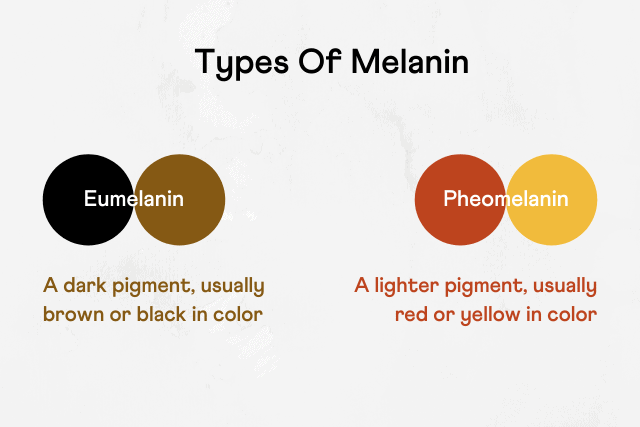
Glutathione has been speculated to be used by the late Michael Jackson to achieve his fair skin. It is a powerful antioxidant but has also shown anti-melanogenic properties. Various mechanisms of action have been considered to explain this property, one of them being the skewing of the melanin synthesis pathway toward the production of lighter pheomelanin instead of darker eumelanin, consequently producing a lightening effect.
I found a research paper published in 2022 looking at supplementation with L-Cystine and L-Glutathione in 124 Asian women for 12 weeks. It showed significant reduction in the size of facial dark spots and overall lightening of the skin. The recommended dose was 500mg L-Cystine and 250mg L-Glutathione.
I recommend L-Cysteine by Epigenar and Glutathione by Goldman Laboratories. You can purchase these from The Natural Dispensary which you can get a 10% discount with the code TLOONG10.
6. Prescription oral tranxexamic acid (TXA)
You may have heard of using TXA to treat melasma.
TXA is commonly used to treat heavy menstrual bleeding. It works by blocking the breakdown of blood clots which prevents bleeding. It has been used in different formulations off-license to treat melasma.
It is proposed to reduce pigmentation by preventing melanocyte activation due UV light, hormones and injured keratinocytes. It’s also proposed to reduce inflammatory a chemical compound called prostaglandin (also found to cause contractions in the uterus) and reduce angiogenesis (formation of new blood vessels) in the skin.
TXA is available in different formulations including tablet, injection, and topical application. TXA tablets are available for oral use in the strengths of 250 mg and 500 mg. Despite several published studies, and its use off-label in clinical practice currently, there is no consensus or published guideline for use of TXA in melasma.
From a review paper of 25 clinical studies published between 2012 and 2022 involving more than 2000 patients, the conclusion was:-
- oral TXA 250mg twice a day seems to be promising treatment option.
- minimum of 3 months treatment is required to see results.
- oral TXA can be used as a mono therapy or with other modalities.
- patients with hypersensitivity to TXA should not receive this treatment.
- women who are on combined hormonal contraception should not be treated with oral TXA.
- Anyone who has active or history of thromboembolic disease e.g. a DVT in the leg or PE in the lung.
FINAL WORDS
As you can see my Glowing Goddess, there are different modalities to improve pigmentation. Often a multiple approach is required as pigmentation can potentially return.
I hope you found this blog useful. I hope to add to it when new treatments come to light.
In my practice, I help my patients have clearer, brighter skin through skincare planning, physical resurfacing, skin boosting treatments and wellness programs to balance hormones and reduce inflammation.
If you like my approach and would like help to achieve a more radiant complexion, please get in touch with my team at [email protected] to book a consultation.
Until the next blog, here’s to glowing skin inside out.
Dr Terry

